Sharp, intense lower back pain when you bend down to pick up something from the floor that leaves you feeling stuck in that position. It feels as if your lower back is simply going to ‘give out’ and you won’t be able to come back up. The only way you can straighten up again is if you push yourself up with your hands on your thigh and knees. The thought of picking up something heavy worries you because your back feels weak and unstable. This is what a spondylolisthesis or spondylolysis feels like. These words sound complicated, but what it means is that one of the bones in your spine (vertebra) slides forward on top of the other. It can also be called an anterolisthesis.
It sounds very serious and scary to have one of the bones in your spine ‘shift out of place’. However, in most cases, people walk around with this condition for years and don’t even know about it and it isn’t something that needs to be fixed with surgery straight away. What is important, is to improve the stability of your lower back, because instability is the main thing that will cause your pain with this condition. This will improve your lower back pain immensely and give you the confidence to bend down or pick up something heavy without thinking twice. Let’s discuss how you can do that.
The structure of your lower back
Let’s first look at the structure of your lower back so that you can understand how a spondylolisthesis will affect you.
The bones in your spine
Your lower back (lumbar spine) is formed by bones (vertebrae) stacked on each other. There are five lumbar vertebrae, called (L1-L5), and five sacral vertebrae, called (S1-S5). The five lumbar vertebrae are stacked on top of each other, like wooden blocks, and they are able to move. Whereas the five sacral vertebrae are fused together, like lego, and moves as a unit.
The vertebrae are not shaped like square wooden blocks, but resemble the shape of oxtail bones. They fit snugly on top of each other, like a 3D puzzle. If you look at it from the top, each vertebra has three parts:
- In the front you have the vertebral body – Large and thick to help carry weight
- In the back you have the vertebral arch – Designed to form a ‘tunnel’ or canal, where your spinal cord and nerves can run through
- Towards the sides you have bony transverse processes – Designed to enhance movement and muscles can attach to these processes
It is important to take note of the vertebral arch, as this is the part that will be affected by a spondylolysis and spondylolisthesis. The vertebral arch consists of:
- 2 Pedicles
- 2 Laminae
- 1 Spinous process
- 2 Transverse processes
- 4 Articular surfaces
The curve in your spine
Viewed from the side, your lumbar spine is curved forward. This curvature, called the lumbar lordosis, is normal. Without the curves in your spine, your spine would have been as straight as a broomstick. Now, imagine bending forward or backward if you had such a straight spine. Your movements would also be very stick-like.
Discs, ligaments, and nerves
Between each vertebra, there is a disc, made up out of a gel-like material. These discs act as shock absorbers when you walk, run and jump. They are responsible for increasing the available movement of your spine, without sacrificing the supportive strength of your vertebral column.
Inside the vertebral canal, you can find your spinal cord that runs all the way from your brain to your lumbar and sacral vertebrae. This thick cord of nerves connects your brain to the nerves in the rest of your body. Nerve roots branch out from your spinal cord and exits in between each vertebra.
To aid in the stability of our 3D block tower, numerous different ligaments connect one vertebra to the next. They criss-cross from one bone to the next, making sure each vertebra stays in place.
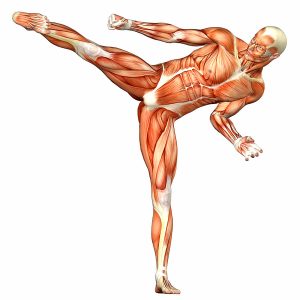
Lower back muscles
The muscles in your lower back can be divided into four groups moving your lower back in four directions (backward, forward, sideways and turning sideways)
- Extensors: Extensor spinae, spinalis Iliocostalis and multifidus
- Flexors: Rectus abdominis, external obliques, iliopsoas, internal obliques and transversus abdominis
- Lateral flexors and rotators: Quadratus lumborum, external obliques, internal obliques and intertransversarii

Stabilising muscles and mobilising muscles
- Stabilisers (stabilising muscles): These muscles can be found in deep layers of tissue, attaching directly onto the lumbar spine (vertebrae). Therefore, they can exert a segmental stabilising force, meaning they can directly stabilise the lumbar segment of your spine. They activate before you even move, so that your spine is already stabilised as you start moving. Throughout the day, they stay activated and contract at a low intensity, making sure that each vertebra stays in place. Overall, if each vertebra is stable, your whole lumbar spine segment is stable. In the end, instability is what leads to injury. These muscles are also called local muscles or local stabilisers, because they connect only to your lower back.
- Mobilisers (moving muscles): Big, strong muscles responsible for moving your upper body/trunk. These muscles cross multiple segments (connecting different parts of your body) and do not attach directly to the vertebrae. They are also called global muscles or global mobilisers, because they don’t only connect locally to the lower back. Their job is to generate a lot of force, move your spine and give you the necessary strength to pick up something heavy.
Take note: Stabilisers and mobilisers work together and help each other out. That means that stabiliser muscles will also help you with movement and global mobilisers will also help you with stabilisation.
What is your core and where does ‘core strength’ come in?
Your core can be described as all the muscles around your middle (the core of your body). It forms a protective cylinder around your lumbar spine that helps to keep it stable. The main core muscles are your diaphragm, pelvic floor muscles, transversus abdominis and multifidus.
The term ‘core strength’ is a term we all know, and most people think that a weak core is why they get lower back pain. However, core strength or core stability is actually your body’s ability to control the core during movement.
This includes using the core muscles while also using stronger mobilising muscles like your iliopsoas, gluteus muscles, quadratus lumborum and rectus abdominis. Good core stability is using the right muscles at the right time with the right intensity to control your lower back during the task at hand. So, not only “static” holding is important, it’s the harmony of the symphony of muscles that need to contact in unity to produce movement.
What is the function of your lumbar spine?
- The vertebrae in your lumbar spine protect your spinal cord and nerve roots.
- Vertebrae in your lumbar spine are the biggest and thickest, because together, they greatly support the weight of your entire upper body.
- They give structure to your lower back.
- Together, the lumbar vertebrae provide stability. Enough stability to withstand something like picking up a heavy weight or a heavy box.
- Your lumbar spine allows you to move and bend your upper body in different directions.
- It connects your upper body to your hips and legs.
The complex anatomy of your lower back is a remarkable combination of these strong vertebrae, linked by strong ligaments, large muscles, and highly sensitive nerves. If you look at the sheer size and solid stability of your lower back, would you be surprised to hear that it is the part of your spine that is also the most flexible?
Extreme opposites
The lumbar spine is flexible enough to allow a gymnast to do back-bends, but also strong and stable enough to allow a weightlifter to pick up extremely heavy weights. Your own lower back allows you the flexibility to bend down to play with your child, while also providing the strength and stability to pick up and carry your child.
The combination of stability and mobility is what makes your lumbar spine so remarkable. Unfortunately, when you have a spondylolisthesis, both the stability and mobility of your lower back will be affected. Then, the thought of bending down becomes impossible.
I have a spondylolisthesis. How did it happen?
The word spondylolisthesis is derived from two Greek words: spondylo which means vertebra (the bones of your spine) and listhesis which means translation (movement). So, spondylolisthesis describes the abnormal movement of one vertebra on top of another.
It starts with spondylolysis
Spondylolysis is defined as a stress fracture in the pars interarticularis of the vertebral arch. It basically means that there is a stress fracture in the piece of bone that connects the vertebral body and the vertebral arch together. A stress fracture or defect in the bone will weaken the strong structure of the bone. Lumbar vertebrae are especially vulnerable to spondylosis with repeated extension and rotation movements. Think of a cricket bowler. First he runs to the cricket pitch, then arches his back and leans backwards, after which he rotates his body and arms and ends with a powerful bowling movement. Whilst bending backwards and rotating your upper body, your vertebrae are compressing against each other. Now, imagine this same cricket bowler practicing his bowling technique over and over. Doing this movement repeatedly and with enough force leads to a stress fracture.
A spondylosis will cause lower back pain and stiffness that usually feels worse on one side. This condition can be managed very effectively if it is caught early enough. However, if it isn’t diagnosed correctly, the spondylosis stress fracture could lead to a full fracture, that leads to the vertebra shifting out of place.
It leads to spondylolisthesis
Spondylolisthesis is the term used when one vertebra moves out of place on top of another vertebra.
- Anterolisthesis: One vertebra slips forward on top of the other. This is the most common type of spondylolisthesis.
- Retrolisthesis: One vertebra moves backward in relation to the other.
If there is a defect or stress fracture in one of the vertebrae in your spine, it will be able to slip out of place. The normal curve (lordosis) of your lumbar spine and gravity then pulls the upper vertebra forward on the bottom vertebra. This causes severe instability of your spine, because a lot more movement takes place than would be allowed under normal circumstances. Usually, a spondylolisthesis will happen in the lumbar spine, but can in rare occasions happen in cervical (neck) vertebrae. The most common levels to develop this pathology is between L4/L5 or L5/S1 vertebrae. These levels greatly help to carry your upper body’s weight.
It ultimately leads to instability
Think of the tower of wooden blocks again. If the blocks are stacked neatly on top of each other, the tower stands on its own. If you push one of the blocks out, the whole tower becomes wobbly. Push the block even further and eventually the tower topples over. The same happens in your spine if one vertebra moves out of place.
It starts out with stiffness, discomfort, and a feeling of “something is not right in my back”. This is your warning sign of a deeper, more complex problem and your body is trying to bring it to your attention. Instability causes increased pressure on sensitive structures like intervertebral discs, joints and nerves, leading to injuries like a bulging disc or nerve compression. Injuries like these will always be accompanied by lower back muscle spasms. We call this muscle guarding. Muscles are protectively guarding the injured site by forming painful spasms in your lower back. in an attempt to protect your spine.
Causes of spondylolisthesis
- Degenerative spondylolisthesis: Occurs from degenerative changes in the spine without any defect in the pars interarticularis. It is usually related to combined facet joint and disc degeneration and ligament weakness that leads to instability and forward movement of one vertebral body relative to the adjacent vertebral body.
- Isthmic spondylolisthesis: Occurs due to a defect in the pars interarticularis. Mostly happens due to microtrauma that takes place in your adolescent years and is related to sports such as cricket, wrestling and gymnastics, where repeated lumbar extension occurs.
- Traumatic spondylolisthesis: Occurs when there is a complete fracture of the pars interarticularis after a traumatic injury like a fall or motor vehicle accident.
- Pathologic spondylolisthesis: This happens due to systemic conditions or bone and connective tissue disorders. This includes bone infections and tumors that directly damage the structure of your spine.
Symptoms of spondylolisthesis
How severe is my spondylolisthesis?
The Myerding Classification is used to classify the severity of your spondylolisthesis. It can be graded according to how far the top vertebra has moved or shifted on the vertebra below it. If a vertebra shifts forward, it is called an anterolisthesis and if it shifts backward, it is called a retrolisthesis.
Myerding Classification
- Up to 25 % ‘shift’ – Grade I spondylolisthesis
- 25 – 50 % ‘shift’ – Grade II spondylolisthesis
- 50 – 75 % ‘shift’ – Grade III spondylolisthesis
- 75 – 100 % ‘shift’ – Grade IV spondylolisthesis
- A grade V spondylolisthesis is called a spondyloptosis. This is the most severe form of spondylolisthesis. This means that the vertebra has shifted out of place completely and it is not even toutching the vertebra above or below it anymore. This can only be caused by a severely traumatic injury like a fall or a motor vehicle accident.
Not everyone will have the same symptoms
Each person is different, and so each person will have different symptoms if they have a spondylolisthesis. Sometimes, it can go unnoticed and someone can walk around for years without knowing they have an anterolisthesis or retrolisthesis. You might just feel like your back is not as strong as it used to be. With time you notice that something isn’t right and your back feels ‘weak’.
A good way to determine how bad your spondylolisthesis is, is to look at how much it is influencing your life. Are you able to bend, sit, get up to stand, walk, run or exercise? The main problem with a spondylolisthesis is instability of your spine, no matter the grade. Instability leads to increased pressure and compression of the joints, discs and nerves in your lower back. This will cause protective muscle spasms in your lower back, because these muscles are contracting even harder in an attempt to keep your lower back stable.
With time, you will become afraid of doing certain movements, like bending forward. You never know when your back will seize up. Now, you think twice before you pick up a box or before you say yes to jump on the trampoline with your kids. Instability and pain in your lower back is so disabling that you won’t trust your back to hold out even with something as simple as bending over to put on your shoes.
It gets worse when there is nerve or spinal cord compression
Your spinal cord is safely protected inside your spine. So, if a vertebra shifts out of position, whether it shifts forward (anterolisthesis) or backwards (retrolisthesis), it will put pressure on your spinal cord. Initially, with a grade I spondylolisthesis, it might not be enough to cause any dangerous compression, but the further the shift, the more dangerous it will become.
Compression of your nerves will cause symptoms like pins and needles, numbness or weakness down your legs. Whereas compression of your spinal cord will cause you to lose control of the strength and coordination in your legs or to lose control of your bowel and bladder.
Continued compression of your nerves or spinal cord can cause permanent damage and permanent weakness. Listen to the warning signs that your back is giving you and get the right treatment from the start!
Diagnosis
Physiotherapy diagnosis
Our physiotherapists are experts in human anatomy and movement, with the necessary experience to diagnose a spondylolysis or spondylolisthesis. We fully understand the intricate way your spine moves in coordination with different muscles and nerves. Doing a full clinical assessment and getting the necessary information about your pain is the starting point.
During your physiotherapy evaluation, we will stretch and stress the different joints in your lumbar spine, to determine which one has been injured. We can accurately identify where your spondylolysis or spondylolisthesis came from. We will also test to see if other structures like discs, muscles and nerves are involved.
If we suspect that your spondylolisthesis is causing spinal cord or nerve compression, a neural examination will be done. This includes testing sensation, neural tension, muscle strength and reflexes.
Thorough evaluation makes our physiotherapists the best at diagnosing this type of problem.
X-rays
If we suspect that you have a spondylolysis or spondylolisthesis, an X-ray will be needed to confirm the diagnosis. The x-ray will show if it is an anterolisthesis or retrolisthesis and it will also show the integrity of the surrounding joint. This way the severity of the spondylolisthesis can be classified.
Your physiotherapist will refer you to get x-rays taken if deemed necessary.
Diagnostic ultrasound
Diagnostic ultrasound will not be an effective tool to diagnose a spondylolysis or spondylolisthesis, as it will not be able to get a clear picture at the depth of the bones in your spine. It can however show whats going on in the surrounding soft tissue and can show inflammation, swelling or the presence of muscle spasms.
If you need an ultrasound, your physiotherapist will refer you.
MRI
An MRI scan can image all of the structures in your lower back, including soft tissue, discs, nerves and bones. If your physiotherapist suspects that you have a spondylolysis or spondylolisthesis, it will first be confirmed with an x-ray. If the x-ray is unclear or if you have neurological symptoms like numbness, weakness or loss of bladder and bowel control, you will need an MRI.
This is an expensive test and you need to be referred by a specialist to get it done. Your physiotherapist will refer you to the right specialist if deemed necessary.
Why is the pain from my spondylolisthesis not going away?
Spondylolisthesis is a deformity in the structure of spine. We cannot reverse the process or change it back to how it was. However, we can help you to understand what is going on in your body, what to avoid and what to do to help yourself.
This is something that won’t just go away on it’s own, so if you keep on pushing through your discomfort, pain and instability, it won’t get better. If you can’t move and bend fully and with ease, your muscles become weaker, joints become stiff and your spine less stable. You become stuck in a cycle of pain, not knowing if it is safe to move or not.
Make sure you are getting the right treatment from the start
The sooner you get the right diagnosis, the better. Certain treatments like medication or wearing a back brace might ease the pain, but it won’t improve the condition of your spine. It will actually lengthen your recovery process. Improving the stability and strength of your spine is the best way to improve your symptoms and protect your spine in the long run.
There is a risk of more critical and possibly irreversible damage to your back, spinal cord and nerves if you don’t take the warning signs seriously. If you are worried about the symptoms you are feeling, rather get it checked out and get the right treatment from the start.
What NOT to do
What you SHOULD do
Making your symptoms WORSE
Problems we see when patients come to us with a spondylolisthesis
Waiting too long and not getting a proper diagnosis
Often, patients wait too long before they seek help. By the time patients come to us for treatment, they have had lower back pain and problems for months or even years. The problem with this attitude is that by the time you come to see us, the problem is a lot more advanced and it will take a lot longer to get better.
If you don’t get a proper diagnosis from the start, it wastes time. If anyone treating your lower back pain is not looking for the cause, they will keep on treating the incorrect thing. This is ineffective and the pain will simply return. Over time, you start to think twice about doing the things you love like gardening or playing with your kids, because you anticipate that you’ll have pain. The longer you wait, the bigger your chances of causing permanent damage.
Trying out, but not completing different forms of treatment
Often, patients try to get relief by taking medication in the hopes that it will ease their pain. They also try massages, foam-rolling, cupping or stretching. However, these treatments only mask the pain and stiffness that comes with a spondylolysis and spondylolisthesis. You are not addressing the root of the problem by trying any of these treatments in isolation.
Wearing a brace to ‘support’ your back will also not be a good form of treatment. The brace might be giving you the stability that you feel you need, but once you take it off, you simply feel weak and sore. Wearing a brace long-term is a big problem, because you could get dependent on it.
And then, a lot of people tend to feel that their lower back pain is easing halfway through their treatment program, so they stop. You need to address the root of the problem and and get your core stability and local stabilisers stronger to handle more load, to improve the stability in your lower back. That is the best long-term solution. Patience is key.
Resting too much or too little
Resting too much leaves you weaker than before. Moving too much causes extra pain, spasms and inflammation. Finding the balance between resting and doing safe movements is key!
Let us help you get the right treatment for your spondylolisthesis and stop it from bothering you again in the future.
Physiotherapy treatment
We can provide the best treatment for a spondylolysis or spondylolisthesis. We understand that you would want to pick something up without any fear of ‘spasming up’ or do a deadlift in the gym with confidence. That is why we are here to provide guidance and answers. Physiotherapists can implement a very effective and structured plan of action that treats all the aspects of your lower back pain and instability. Our physiotherapy treatment will help you to improve your muscle strength so that you are able to regain stability and restore normal movement of your lower back.
Physiotherapy will be aimed at relieving acute pain and strengthening the muscles around your spine. Like enhancing your own internal corset/brace. Because the problem is caused by a structural deformity, that we cannot change, the aim will be to help you manage your symptoms, get you stronger and teach you which activities to avoid. .
The basic structure of our treatments:
- Determine what has been injured
- How badly is it injured?
- Protect it from further injury
- Give it time to heal
- Strengthen
- Re-evaluate to monitor progress
We will be looking at different aspects, like testing your lower back’s ability to bend and turn in different directions. And we will also look at muscle strength, range of motion, flexibility and stability. Treatment will include: soft tissue massage, joint mobilisations, dry needling, strapping, laser therapy, nerve mobilisations and guiding you through a rehabilitation program of gradual strengthening, control and conditioning. It’s important that you commit to the treatment plan, as this improves your chances of successful long-term recovery.
Phases of rehabilitation
1st Phase: Protection and initial healing
Protect
Patients tend to push through their pain and even continue to exercise with severe lower back pain. This can cause continuous inflammation and pain. Protect the injured area by resting and avoiding painful movements.
Avoid anti-inflammatory medication
Avoid using anti-inflammatory medication if possible as it delays healing. Ideally, use only pain medication without an anti-inflammatory component in the initial phases of your injury. That way, your pain will be under control, and with time you can taper off and stop taking the medication completely.
Compression and heat
Strapping can provide good temporary support for the painful area in your back, which in turn will decrease your pain.
Information
Make sure that you get information from the person that is treating you. Its important to understand what you should and shouldn’t do. If you are informed, you can also make the right decisions. Your body knows best, so avoid too many types of treatments at once.
Load
Let pain guide you to gradually return to your day to day activities. Initially, it is tricky to know if it is better to rest or to move, but finding a balance between the two is the best you can do. Safely moving your back, allows the joints and muscles to move, without you overdoing it.
2nd Phase: Establish pain free range of movement
During your examination, it will become clear what you are able to do, and what you should avoid. When doing a movement, like bending forward, you will be able to move to a certain point, before your pain starts. This is your pain-free range of movement. You are safe to move in this range and our exercises will be targeted between these boundaries of your pain.
The aim is that, with time, your pain-free range of movement improves do that you’re able to bend down as far as you would like to.
3d Phase: Tissue healing
We monitor the progress of healing in your spine and surrounding muscles and will make sure that tissue healing is on track. On a cellular level we’re able to accelerate tissue healing using dry needling, laser and ultrasound. As healing takes place, we want to see not only improvement of your pain, but also improvement in the control of your spine and your muscles’ ability to endure contractions. If optimal healing takes place, then your spine will be able to move more freely and the muscles in your lower back should be able to contract and relax smoothly without any pain.
4th Phase: Regain stability
During each session we will re-evaluate you to see if your lower back can handle moving in different directions, and if you are able to maintain the stability of your spine with the surrounding muscles. An important starting point is to help you find a position where you feel your spine is in a neutral position. Often, just getting used to keep your spine in a stable and neutral position is hard work because you got used to wrong movement patterns. From here on, you will have to be able to hold the stable position of your spine while we slowly get you to do different exercises. This way, you build your muscle strength back up with the ability to keep your spine stable. The best foundation you can have.
5th Phase: Full range of movement
The most important component of your rehabilitation is to regain full range of movement of the your spine and the muscles around it. You should be able to bend in all directions. During this phase we will use: massage, stretches, myofascial release and joint and neurodynamic mobilisations.
6th Phase: Muscle strength
It’s common to feel some pain when you start to work on muscle strength. This is could be due to abnormal muscle tissue adhesions which prevents the muscle from contracting smoothly. But it could also be due to poor endurance and muscle strength. You’ll feel lower back muscle pain if your muscles start to fatigue. That’s why it is so important for you to strengthen the muscles around your spine. Ultimately, it improves your pain and gives your spine the necessary stability so that you have a stable foundation. Your posture will improve and doing your day to day activities will become easier. During this phase of rehabilitation we will progress your exercises more and more, adding resistance, doing more repetitions and building your overall strength. You should pick up something heavy with more confidence after completing this phase
7th Phase: Muscle control and core stability
It is one thing to feel your muscles get stronger, but another thing to do movements with control. The type of muscle contraction we use during this phase of rehabilitation is called eccentric muscle contractions. Muscles are able to contract and shorten concentrically, but they are also able to slowly lengthen eccentrically. You must be able to keep your spine stable whilst moving it, needing control and stability. You should also be able to control your spine while you move other body parts like your legs or arms. Improving your core stability will be a big part of this stage of rehabilitation. With improved muscle control, you improve the stability of your spine, thus protecting it and decreasing the chances of recurring symptoms of a spondylolisthesis.
8th Phase: Testing for return to activity
Gradually returning to your routine and getting used to the intensity of your usual activities is a big part of your recovery. This way, we can determine if you are ready to return to fully working and training without any painful flare-ups. The improved stability of your spine is like a stable base or foundation that you can move from. Even with repetitive movements throughout your day (like sitting and getting up) or more load (like picking up your child), your back muscles should be able to handle it while keeping your spine stable. Your physiotherapist will guide you to re-engage in safe increments, and make adjustments where necessary.
9th Phase: Power and speed
You need to be able to do certain activities like sprinting or deadlifts with high load and speed. The muscles in your back must keep up with the demands of your body. During this phase your physiotherapist will guide you to challenge your muscles past your normal boundaries to determine how your body reacts to different forces. Ultimately we prepare you to return to participating in your sport.
Whatever must be done – we’ll get you there. Weightlifting, sprinting, jumping, golf swings and much more.
10th Phase: Sport Specific Training
This is the final stage of rehabilitation. Your physiotherapist will still continue with myofascial release, trigger point release and electrotherapy modalities where needed, but sport rehabilitation is most important during this phase.
Depending on your sport, your physiotherapist will tailor specific exercises that will help strengthen the muscles pertaining to your sport. A successful outcome is when you can participate at full power and speed, not to mention the benefits of minimizing your chance of recurring back muscle spasms.
Healing time
Acute pain may be due to a new activity or excessive exercise and this causes inflammation around the vertebrae. Acute pain should settle in 2 – 4 weeks with treatment. It will take at least 6 weeks for healing to take place together with the settling of your symptoms. Remember that spondylolisthesis is a structural deformity. Physiotherapy can help to relieve pain, but it cannot change the structure of your spine.
Depending on the severity of your symptoms and initial inflammation, you will need physiotherapy treatment twice a week for the first two weeks. After this, your treatment sessions can be spread out to once a week or once in two weeks. You only spend an hour at a time with your physiotherapist. How fast you recover will greatly be up to you. If you complete your physiotherapy treatment protocol, you should be able to recover completely and return to your sport.
Other forms of treatment
- Your doctor will probably prescribe anti-inflammatory medication or give you a voltaren injection to get the muscle spasm to ease. Both of these medications will give temporary relief to the pain and stiffness that you are experiencing. However, it will not be the solution to your problem. Once the effect of the medication wears off and you try to get back to working or exercising, your pain could simply return.
- Cortisone injections could ease some of the pain and inflammation in the joints of your spine, but it is not a good form of treatment for long-term use. It weakens the integrity of the joints and ligaments in your spine.
- Getting your back ‘aligned’ or ‘clicked’ in the hopes of improving the lower back pain will not improve or take the spondylolysthesis away. Your back is already unstable, a manipulation could worsen this instability and worsen your injury.
- A biokineticist will be able to help you in the final stages of your rehabilitation or to get you back to actively training for your sport.
- Wearing a back brace in the hopes of giving it extra stability might ease your back pain and make you feel better while you’re wearing it, but it won’t be the solution to your problem. In fact, muscles become weaker when you wear a brace and you become dependent on the brace. It will only worsen your problem.
- Stretching or foam-rolling your back might ease your lower back muscle pain temporarily, but if the real problem isn’t addressed, the pain will simply return.
Is surgery an option?
Non-surgical treatment for spondylolisthesis is the first choice. If this fails a fusion of the vertebrae may be considered. The goal of the fusion is to stabilize the affected part of the spine, decompress (give more height) and repair alignment. This is very invasive and requires 6 weeks of recovery afterwards, after which it will take another 2 – 6 months to get you back to your normal routine and exercise.
What else could it be?
- Disc bulge/herniated disc: This causes pain in your lower back, with the possibility of pain spreading down your leg. It is especially painful when you bend forward, sit, or drive.
- Spondylolysis: A stress fracture of the pars interarticularis in the vertebral arch, with no displacement of the vertebrae, can be the precursor of spondylolisthesis. It causes pain and instability in the lumbar spine.
- Sacroiliitis: A dull ache in your lower back and buttock aggravated with sitting for a long time.
- Lumbar spondylosis (Osteoarthritis) is pain caused by degeneration in the joints in your lumbar spine. The pain feels worse when you overdo it by walking too far, standing too long, or sitting too long. It also feels worse in cold weather and in the mornings but better when resting.
- Lower back muscle spasm: Muscle pain and stiffness in your lower back. It is usually caused by doing something strenuous like picking up a heavy box, but it could also be a sign of muscles guarding a deeper problem in your back. It is painful when you bend, get up, or turn, and better when you rest.