Hip Bursitis is inflammation of the bursae found in your hip. A bursa is a small fluid-filled sac or gel-like cushion that reduces friction between a bone and soft tissues surrounding it. When a bursa becomes inflamed, it is called ‘bursitis’. This condition occurs when the bursa becomes irritated, compressed or infected. Greater trochanteric bursitis is the most common. It mainly causes pain over the side of your hip, right over the knob of your hip where you can feel your hip bone. A well known symptom of hip bursitis is pain when you lie on your side.
Such a small structure can cause you a lot of pain and problems if the root of the problem isn’t addressed. It is important to get the right treatment for your hip bursitis as soon as possible to avoid long recovery periods.
Anatomy of your hip bursae
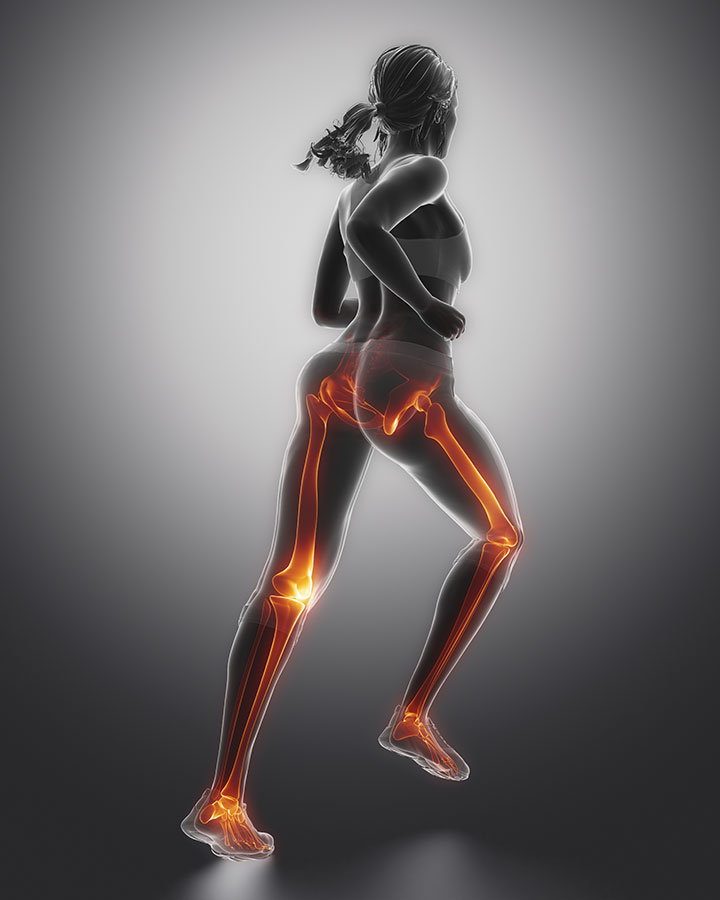
Your hip joint consists of your femur (thigh bone) fitting into the socket of your pelvis. Many other soft tissue structures cover the hip joint like ligaments and muscles, and bursae. A bursa is a thin, slippery sac filled with a small amount of fluid. The type of fluid found in a bursa is called synovial fluid. This is the same kind of fluid found inside joints in your body. It is rich in proteins that provide nutrients to the membrane of the bursa. There are hundreds of bursae in your body, all located close to different joints in your body. The bursae around your hip is separated significantly from the actual hip joint by soft tissue and bone. Thus, hip bursitis is not a cause of true hip joint pain.
Bursitis
The term bursitis is used when the membrane of the bursa becomes irritated and inflamed. The inflamed membrane then produces excess synovial fluid, causing the bursa to swell. Because the different hip bursae are located underneath layers of skin, fat, muscle, and other soft tissues, even moderate to severe swelling will not be visible from the outside.
There are three major bursae found around the hip:
- Iliopsoas bursa: This bursa is located near the groin, underneath the iliopsoas muscle. If this bursa becomes inflamed, the condition is called iliopsoas bursitis and it will typically cause pain more towards the front of your hip/groin.
- Ischial bursa: This bursa is located on the pelvis bone, in your lower buttock area. Right in the fold that your buttock forms, where muscles like your hamstrings attach. If this bursa becomes inflamed, the condition is called ischial bursitis or ischiogluteal bursitis. It will typically cause pain toward the fold of your buttock.
- Trochanteric bursa: This is large bursae that lie over the bony knob (greater trochanter) at the top of your femur. This is the hip bursae that is the most prone to bursitis and when the term hip bursitis is used, it mostly refers to greater trochanteric bursitis (also known simply as trochanteric bursitis). This condition will cause pain towards the outer side of your hip.
With Trochanteric Bursitis, two bursae are commonly involved:
- Subgluteus Medius bursa – located above the greater trochanter and underneath the insertion of the gluteus medius muscle.
- Subgluteus Maximus bursa – located between the greater trochanter and the insertion of the gluteus medius and gluteus maximus muscles.
Another important soft tissue structure to take note of, is the iliotibial band (ITB). This is a fibrous, tight band of tissue that runs from your the greater head of your femur down to the side of your knee. Your ITB provides extra stability as it connects your hip joint and your knee joint. However, the movement and friction between the head of your femur bone and your ITB can contribute to the irritation and inflammation of your trochanteric bursae.

What is the function of a hip bursa?
The purpose of the bursae found in and around your hip joint, is to reduce friction between the bones and the surrounding soft tissue, such as skin, muscles, ligaments and tendons. It prevents soft tissue like muscles or tendons from getting injured as they slide over the hard surface of a bone and this allows smooth movement. A bursa forms a sort of cushion to minimize friction and it helps to absorb shock with certain movements or with impact against your hip. The trochanteric bursae also help to decrease the friction caused by your ITB when it rubs over the head of your femur with any hip and knee movements.
Think of a piece of soft leather that gets rubbed over a sharp corner of a table. Over time, a hole would form in this piece of soft leather. Now, compare this to your own hip. If there was no bursae, your muscles and tendons would wear out by rubbing over your hip bone all the time.
How does hip bursitis happen?
Bursitis occurs when the membrane of the bursa becomes irritated and inflamed. This causes an excess in the production of synovial fluid, causing the bursa to swell. When the bursa becomes swollen, it will influence the normal movements of especially your gluteus (buttock) muscles and tendons as well as your ITB. Now when these muscles are contracted, it is painful and your movement becomes limited. Repetitive movement/friction of the muscle or tendon scraping over the bursa, causes the bursa to stay swollen.
Trochanteric bursitis
This is inflammation of the trochanteric bursae. You can compare the trochanteric bursa to a swollen water balloon and the buttock muscles and ITB to ropes, strapped over this water balloon. These ropes are pulled in different directions and this puts more pressure and compression on an already swollen water balloon. The same happens with trochanteric bursitis. Inflammation of the bursa starts to irritate other structures around as well and this keeps the cycle of pain going. This is why something as simple as lying on your side or climbing stairs causes you hip pain.
The process of inflammation
The fact that it’s called bursitis implicates it has an inflammatory component, but we have to take into account that some of the typical elements of inflammation are not actually present with a typical case of hip bursitis. The 4 elements of inflammation are: pain, swelling, redness and heat. Because the hip bursae are located deep beneath other layers of tissue, you don’t typically see swelling, redness or heat. The only cardinal sign of inflammation that you can go on, is pain.
Inflammation of the bursa is a slow process, which progresses over time. Trochanteric bursitis most often occurs because of friction, overuse, direct trauma or too much pressure. Hip bursitis can be acute due to an injury or trauma, but it can just as easily become chronic.
Chronic hip bursitis
Overuse, extreme movements or muscle strains contibute to chronic trochanteric bursitis and can often lead to ‘Greater Trochanter Pain Syndrome’ (GTPS). The name of this condition is often used as a general term to describe pain around the greater trochanteric region or side of the hip. Trochanteric bursitis is frequently confused with GTPS, but is in fact only a component of GTPS. Other conditions like ITB syndrome also contribute to GTPS. When the pain caused by your throchanteric bursitis becomes chronic, you end up in a vicious cycle of pain and this causes weakness, stiffness.
Take note: Trochanteric hip bursitis cannot simply happen out of its own. Overuse and repetitive friction are the main things to look at. This means that any treatment for hip bursitis cannot simply treat the inflamed bursa. Taking a step back and getting to the root of the problem is the only effective way to treat trochanteric hip bursitis.
Septic bursitis
There is a very small and rare chance that you could have septic hip bursits. Septic hip bursitis happens when a bursa in the hip area is infected. It is a potentially serious condition that requires medical attention and treatment with antibiotics. Septic hip bursitis will cause similar symptoms to aseptic (non-infectious) bursitis, as well as fatigue, fever, warmth and redness at the hip, and/or an overall feeling of being ill. Recognizing the symptoms of septic hip bursitis can lead to quick and appropriate treatment.
Causes of hip bursitis
Usually, there is a trigger that sets off the initial inflammation response to cause trochanteric hip bursitis. A bump or a fall directly onto your hip that you thought nothing of. However, this is just the start. Repetitive movements then keep you in a cycle of constant swelling and irritation of your bursa.
- Repetitive friction between the bony point of the femur (greater trochanter) and the soft tissue around it
- Stiffness of the hip joint (caused by conditions like arthritis)
- Going up and down many flights of stairs every day
- Activities with repetitive hip movements like cycling, climbing or running
- Repetitive contraction of buttock (gluteus muscles) like running or climbing up a hill
- Unequal leg length
- Posture and position of your pelvis and lower back
- Weakness of hip and buttock muscles (especially weaker on one side e.g recovery after having a stroke or other injuries)
- Lying on your hip/side for a prolonged period (e.g. bedrest)
- Sitting on a hard surface for extended periods of time
- Sports that involve a lot of running, twisting and changes of direction when your full weight is on the leg (hockey, cycling, running and athletics)
Symptoms of hip bursitis
How bad is my hip bursitis?
There is no grading system to grade the severity of your hip bursitis. The impact that it has on your life and exercise or sport will be the biggest indicator as to how much it is affecting you.
- Acute hip bursitis occurs because of trauma or a massive overload. After a few days symptoms like pain, swelling and a warm feeling when touching the affected area can be noticed. It will also be very painful to move your hip joint.
- Chronic hip bursitis is caused by overuse, too much pressure on the bursa or even a gluteus muscle strain/fatigue. The main symptom here will be hip pain that seems to decrease when you rest and increase when you move your hip or put pressure on your hip.
With chronic hip bursitis, it becomes harder to distinguish if your pain is coming purely from an inflamed hip bursa. Other structures in the area like buttock muscles and tendons and your hip joint become involved as well. With trochanteric bursitis, it can lead to greater trochanteric pain syndrome (GTPS). This condition is simply used to describe and include different conditions that cause pain over the side of your hip. Now you become stuck in a cycle of pain where you can easily get ITB friction syndrome or even tendinopathy of one of your hip muscles. Rather seek help and get the right treatment when you think you have symptoms pointing to hip bursitis.
Different bursae, different symptoms, different treatnent?
Symptoms of the different hip bursitis’ may differ, but in the end the treatment and management will stay the same, except in the case of septic hip bursitis. Although your chances of getting septic hip bursitis are small, it is a serious medical condition. Look out for symptoms like fatigue, fever and an overall feeling of being ill or feeling ‘off’. It is important to get the right treatment for septic hip bursitis. However, if the right treatment is administered, it will clear up quickly.
Diagnosis
Physiotherapy evaluation
Our physiotherapists are experts in human anatomy and movement with the necessary experience to diagnose hip bursitis very easily. We understand the intricacy of the biomechanics of the hip and we look at all other aspects that could be contributing to your hip pain. Getting the necessary information from you, together with a clinical assessment is the starting point.
During your physiotherapy evaluation, we will stretch and stress different structures around your hip like your ITB, soft tissue around the inflamed bursa, muscles, ligaments and your hip joint itself. We also test muscle strength and length, range of movement and can measure swelling in the area. Another important aspect we will be looking at is your posture and the way your pelvis and lower back moves when you move. This is why our physiotherapists are the best at diagnosing this type of problem.
X-rays
An x-ray of your hip will only show the bones that form your hip joint, so it will not be necessary to diagnose hip bursitis. It will however show fractures or signs of possible hip joint degeneration or arthritis. If your physiotherapist feels that it is necessary for you to get x-rays, you will be referred to the right place.
Diagnostic ultrasound
Diagnostic ultrasound is effective in showing signs of hip bursitis. The trochanteric bursa is located underneath layers of soft tissue and muscles, but not too deep. Thus, diagnostic ultrasound will be able to show signs of increased fluid in the bursa (swelling). Comparing the cross section and size of the bursae on each side, will show if a bursa on one side is swollen or irritated. Doing a follow-up ultrasound after your treatment will show if the swelling has gone down.
Your physiotherapist will refer you to get an ultrasound done, if deemed necessary.
MRI
An MRI is a very expensive type of scan and you can only get one via a referral from an orthopaedic surgeon. Although an MRI will show soft tissue structures, it is seldom necessary to get one if you have hip bursitis. Deep soft tissue structures and structures inside your hip joint will be visible on an MRI. So, if your physiotherapist feels that it is necessary for you to get an MRI to show what is going on deep inside your hip, you will be referred to the right specialist.
I have hip bursitis, why is my pain not going away?
You have had hip pain for a while and got diagnosed with hip bursitis. Initially, you rested for a while and took some anti-inflammatory medication. This seemed to help, but once the medication was finished and you wanted to get back to exercising, you found that your pain did not improve as you would have liked.
Without a proper evaluation and treatment plan, your hip pain won’t simply improve. In the case of hip bursitis, inflammation causes the bursa to swell and this irritates the surrounding soft tissues. If you focus on resting, it will probably help the inflammation and irritation to go down. However, now your hip joint has become stiff and your buttock muscles have become weak. Trying to push through the pain to get back to exercising will simply cause you to strain these muscles that will get tired quite quickly. A sudden increase in movement and exercise will again increase the friction over the trochanteric bursa, and this just starts up the whole cycle of inflammation again. Now you have become stuck in this cycle of pain and you don’t know whether it is better to rest or move.
Which is better? Resting or moving?
With more rest and a change in your day to day routine, the inflammation in the bursa will start to settle. Luckily there won’t be any scar tissue formation in the bursa itself. However, in the time that it took for the inflammation to improve, the buttock muscles and their tendons have become either fibrotic, or thickened or stiff. These stiff buttock muscles are now not able to handle work of continuously contracting and they will fatigue quickly. This adds more pressure on the trochanteric bursa and irritates the bursa again.
The tricky part with hip bursitis treatment, is to find the balance between resting and moving. It is important not to treat only the bursa, but to address the bigger picture of everything that contributes to your hip bursitis. A very important aspect of your treatment should be to get your buttock muscles back to their normal state to contract under load (like you climbing up a step) and trough the whole range of hip movement. This can only be done through a proper rehabilitation and treatment program.
A big problem we see with hip bursitis
Waiting too long and not getting a proper diagnosis
A common problem we see is that patients wait too long before they seek help. By the time patients come to see us, they have had hip pain and problems for months. If you don’t get a proper diagnosis from the start, it will also waste time. If anyone treating your pain is not distinguishing between pain coming from a muscle, joint, ligament or bursa in your hip, they will keep on treating the incorrect thing. This will be ineffective and may aggravate the problem. Now, the pain becomes unbearable and it holds you back. It prevents you from sleeping on your side, getting out of the car or walking far. Because you have waited so long, recovery will take so much longer.
Trying out other forms of treatment
Often, patients try to get relief by taking anti-inflammatory medication or getting a cortisone injection in the hopes of decreasing their pain. This, however, only slows the process of healing. Initially, you will have to take some of these medications to decrease your pain and swelling. You are not however addressing the root of the problem by simply taking medication. The only way to address your pain will be to look at the bigger picture and everything that contributes to your hip bursitis.
Getting a manipulation of your back done to get your hips back in line, won’t help your pain at all. It won’t change the state of the inflammation happening or have a lasting effect.
Resting too much or too little
Resting too much leaves you weaker than before. Moving too much causes extra friction of the soft tissue gliding over the bursa. This leads to increased swelling and inflammation in the bursa. Finding the balance between resting and moving is key!

Physiotherapy treatment for hip bursitis
We are confident that we can provide the best treatment for hip bursitis. We understand that patients are often anxious to get back to their day to day activities, so that is why we are here to provide guidance and answers. Physiotherapists can implement a very effective and structured plan of action that treats all the aspects of the problem and get you back on to where you want to be living your best life. Our physiotherapy treatment plays a vital role to restore the normal slide of the tendon and muscles over the bursa and ensure the bursa does what it’s supposed to do, without flare-ups.
The basic structure of our treatments:
- Determine what has been injured
- How bad is it injured?
- Protect it from further injury
- Give it time to heal
- Strengthen surrounding muscles
- Re-evaluate to monitor progress
We will be looking at different aspects, like testing and measuring your ability to use your hip and leg with activities like climbing up a step or running. And we will also look at other aspects like muscle strength, range of motion, flexibility and stability. Treatment techniques will include: soft tissue massage, joint mobilisations, dry needling, strapping, laser therapy, nerve mobilisations and guiding you through a rehabilitation program of gradual strengthening, control and conditioning of the muscles around your hip. It’s important that you commit to the treatment plan, as this improves your chances of successful long-term recovery.
Phases of rehabilitation
1st Phase: Protection & initial Healing
Protect
We have found that patients tend to continue walking on their injured leg with a limp. That means that your hip and hip bursa still has to carry the load and muscles still repeatedly glide over the bursa every time you step on your leg. Using crutches for a while if your pain is really severe will be a good idea.
Rest
Rest from activities that is worsening your pain. Don’t simply push through pain when you try to exercise and don’t simply continue to lie on your side at night. As soon as your pain starts to improve, don’t test it. This way you won’t flare up inflammation again. Give it time.
Ice
Applying ice, will have a numbing effect on your pain and will help in reducing some of the swelling of the bursa. Take ice cubes wrapped in a towel and apply it to your hip when you lie down. Apply it for the first few days if you struggle with severe swelling and inflammation. Always keep a towel between the ice and your skin (to prevent freeze burn).
Compress
Use strapping or elastic compression bandage to keep the side of your hip supported. The feeling of support helps for the management of pain and protects the soft tissue. Strapping/taping will also help to control swelling.
2nd Phase: Establish a pain free range of movement
During your examination and tests, it’ll become clear which movements you are able to do, and which movements you should initially avoid. We identify what exactly is contributing to the compression force over the bursa in your hip. During this phase it is important to find a good balance between resting (to assist in decreasing the irritation of the bursa) and safe pain-free movement (to keep your joints and muscles mobile). There is a pain free range of movement that you’re safe to move in, and our exercises will be targeted between these boundaries. On completion of this phase you should be able to perform moments within limits of your pain.
As your rehabilitation progress we aim to gain a larger pain-free range of movement while your painful range becomes less intense.
3d Phase: Tissue healing
During this phase of your treatment, we monitor the progress of the inflammation and compression of your hip bursitis. Doing a follow-up ultrasound after a few treatment sessions is a valuable tool. This way we can make sure that the size of the bursa has gone back to its original size and the inflammation has settled. We help to accelerate tissue healing using dry needling, laser, ultrasound and electrotherapy.
4th Phase: Ability of your tissue to handle stress
During each session we will re-evaluate to see if you are achieving the necessary targets for the trochanteric bursa to be able to handle tensile, elastic and compression forces. With every movement, like sitting and getting up from sitting, your bursa will be put under pressure. This happens due to the muscles and tendons that glide over the bursa as you move. It needs to be able to handle this. We use isometric muscle contractions to get the muscles around your hip moving. These are a very safe form of exercise using muscle contractions without momentum to keep the surrounding muscles active without compromising or putting too much compression on your bursa.
5th Phase: Full Range of Movement
The most important component of rehabilitation is to regain full range of movement of the muscle fibers around your hip and of your hip joint itself. Any thickened tissue or scar tissue that formed between the layers of tissue covering your hip bursae, must be lengthened and orientated to allow smooth movement. These layers of muscle and soft tissue must be able to glide over the bursa without irritating it again. During this phase of your hip bursitis treatment, we will be using massage, stretches, joint mobilisations and neurodynamic mobilisations to achieve full range of movement.
6th Phase: Increasing muscle strength
Its common to feel some pain once you start to use the muscles around your hip again. Now that you have improved movement, it is very important to work on strengthening your muscles as well. This way you are able to get back to walking far or exercising without pain. During this phase of treatment, we will start to give you more difficult exercises and add resistance and more repetitions to your exercises. This way your muscles get stronger and are able to endure repeated contractions. When your buttock muscles fatigue, the compression on your trochanteric bursa will increase. Walking, running or climbing stairs requires you to move your whole leg and hip through it’s full range repeatedly. You will need strength and endurance for this.
7th Phase: Stability and control
Different muscle groups around your hip, core, back and knees all work together to give stability to your hip. Muscles can shorten and lengthen according to the activity you do. Working on strength alone, is not enough to improve your hip control and without hip control the compression on your trochanteric bursa will increase. During this phase of hip bursitis treatment, we will be adding elements of balance and doing slow and controlled exercises with eccentric muscle contractions to improve your hip stability.
8th Phase: Testing for return to activity
With time, you will gradually be able to return to your previous day to day activities, work and training. Your physiotherapist will help to determine if the compression and irritation of your trochanteric bursa, has improved enough for you to be able to handle repetitive actions without flare-ups. You will return and re-engage in safe increments, and adjustments can be made where necessary.
9th Phase: High Speed, Power, Proprioception
The trochanteric bursa and buttock muscles around your hip must be able to withstand a high load of friction and compression. During this phase your physiotherapist will guide you to challenge your muscles past the ‘normal’ boundaries to determine how it reacts to different forces. This way, we can ensure that the muscles will be able to keep up with the demand of your body without irritating the underlying bursae. Ultimately we prepare you to return to participating in your sport.
Whatever must be done – we’ll get you there. Jumping, hopping, fast footwork, sprinting and much more.
10th Phase: Sport Specific Training
This is the final stage of rehabilitation. Your physiotherapist will still continue with myofascial release, trigger point release and other manual treatment where needed, but functional sport rehabilitation is most important during this phase.
Depending on your sport, you will get exercises specifically tailored for you, that will help strengthen the muscles you need most for your sport. A successful outcome is when you have gained knowledge throughout the treatment program to understand what was causing your hip bursitis and can participate in your training/sport at full power and speed again. Not to mention the benefits of minimizing your chance of recurring chronic trochanteric hip bursitis.
Recovery Time
Taking into account that the healing process takes about 6 weeks, you will need to allow yourself space within that 6 weeks for recovery. In all but the extreme cases of Trochanteric bursitis, you should recover quickly and be able to return to your sport after you have followed the prescribed treatment protocol from your physiotherapist. Depending on the severity of your symptoms and initial inflammation, you will need physiotherapy treatment twice a week for the first two weeks. After this, your treatment sessions can be spread out to once a week or once in two weeks. You only spend an hour at a time with your physiotherapist. How fast you recover will greatly be up to you.
Other medical treatments for hip bursitis
- Your doctor could prescribe anti-inflammatory medication or give you a cortisone injection as treatment for your trochanteric hip bursitis. Both of these medications will give temporary relief to the pain and inflammation that you are experiencing. However, it will not be the solution to your problem, as it will be a temporary pain relief. Once the effect of the medication wears off and you try to get back into your normal routine, your pain could simply return.
- Getting your hip ‘aligned’ or ‘clicked’ in the hopes of improving the pain and stiffness in your hip will not solve the problem. An alignment cannot change the state of your trochanteric hip bursitis and will not be an effective treatment. You will have to look at the bigger picture and all aspects contributing to your pain.
- Getting insoles to change the alignment of your foot in the hopes of changing your whole leg’s alignment can be a good idea. However, it won’t change the state and symptoms of your trochanteric hip bursitis on its own. You will have to use these insoles in conjunction with a proper treatment plan.
- A biokineticist will be able to help you in the final stages of your rehabilitation or to get you back to actively training for your sport. Your physiotherapist will refer you the right person.

Is surgery an option?
It is very rare that surgery will be an option for treatment of your hip bursitis. Only in the very worst case can surgery be added as an option. The bursa causing pain will be completely removed.
In the case of septic hip bursitis, the fluid in the swollen bursa can be drained out and will be sent for lab tests to see what kind of infection was causing the septic hip bursitis.
If your are thinking of having surgery for hip bursitis, discuss this option of treatment with your Physiotherapist first. Make sure that you do not unnecessarily lengthen your healing process.
What else could it be?
- Hip joint osteoarthritis – Pain and stiffness of your hip that feels especially worse in the mornings and in cold weather.
- Muscle pain caused by a strain or tear of the buttock muscles, quadriceps muscle, groin muscles, or hamstring muscles. This type of pain will feel worse with activity or exercise and better with rest.
- Tendinitis of the quadriceps muscle, buttock muscles, groin muscles or hamstrings. This type of pain typically feels better when you move and worse after exercise or the following morning.
- Pinched sciatic nerve – causing pain, pins and needles, numbness or weakness around the hip and buttock or even down your leg.
- Avascular Necrosis of the Femur Head – deep groin and hip pain that’s constant and progressively gets worse.
- Femur fractures or a stress fracture of the femur head – Hip pain that feels much worse when you take weight on your leg, usually after a fall.
- Lower Back Pain referring into your hip – Pain radiating from your lower back down into your hip and leg. It feels worse when you bend down, try to pick up something heavy or get up after you’ve sat for a while.
- Iliotibial band syndrome – Pain over the side of your hip or down your leg towards the outside of your knee that feels worse during activities like running or walking far.
Also known as:
- Trochanteric bursitis
- Greater trochanteric busitis
- Iliopsoas bursitis
- Ischial bursitis
- Greater trochanter pain syndrome
- Iliotibial band syndrome

