Calf muscle tears, also known as tennis leg, are much more common than you would think. A sudden change of direction or burst of speed is sometimes all it takes to strain your calf muscle. Even more surprisingly, a muscle strain in your calf doesn’t always feel like a tear. In practice, we often find that someone comes in complaining of tightness in their calf muscles, only to find that they actually have a strain or tear. You may feel like you can walk it off or stretch it out, but the bad news is that up to 16% of calf strains reinjure the same muscle again.
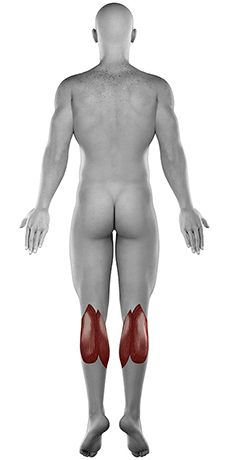
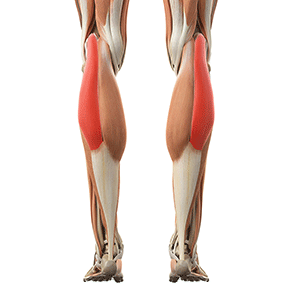
The Anatomy of your Calf muscles
Your calf consists of 2 large muscles – Gastrocnemius and Soleus muscles. Gastrocnemius is more superficial, giving your lower leg that curved look, with Soleus below it, closer to your shin bone.
The Gastrocnemius muscle has two heads (medial – on the inside and lateral – on the outside) and crosses both the ankle and knee joints. This is also called a bi-articular muscle. The fact that is crosses not one but two joints makes it vulnerable to injury , and about 70% of calf muscle tears involve the Gastrocnemius muscle.
Soleus is the deeper of the two, and only crosses your ankle joint. The two muscles run closely together, joining to form the Achilles tendon, which anchors the two muscles to the back of your heel bone.
Both the calf muscles are attached to tendons on each side called the musculotendinous junction. The most common place where a torn calf muscle occurs is at this joining point of muscle and tendon.
What does it do?
The Gastrocnemius muscle is the more superficial calf muscle, and the one you will see contract when you stand on your toes. In other words, contracting the Gastrocnemius muscle causes your ankle to plantarflex. This muscle is more active when you point your toes with a straight knee and also has a lesser role in bending your knee. The Soleus muscle is underneath Gastrocnemius, and only crosses the ankle joint. Soleus also plantarflexes your ankle, but is more active when your knee is bent. Have you ever noticed how often you point your toes? Pushing off with every step needs plantarflexion, as well as climbing a step or getting in your car.
Pointing your toes may not seem like an important job, but the intricate working of your legs make these muscles a lot more important than simply making you taller to reach the top shelf. Both muscles help to control your foot position during walking, running and jumping. Without proper strength and mobility in your calf muscles, you will find that you stumble and miss a step much more often than you’d like.
Why did I pull my calf muscle?
One of the key factors involved in a gastrocnemius or soleus tear is tight calf muscles. Runners are quite vulnerable to calf muscle strains, because the muscles contract at high intensity to push off with each stride. Sports that involve jumping or sudden changes in direction, for example squash, netball or soccer, have an even higher risk for a torn calf muscle. That’s because these activities rely heavily on your calf muscles to propel you off the ground and get that quick burst of speed to get to the ball.
When a muscle needs to contract at a very high rate and force, this overload of ‘pulling’ on the muscle causes microscopic tears in the muscle fibers. A combination of overload while your muscle is stretched, puts your calf muscle fibers under even more strain. Your body reacts to these microtears by activating your nervous system to signal the muscle that it has been injured. Your nervous system reacts by contracting that muscle and increasing the muscle tension. This increased muscle tension is why you feel tightness or even cramping in your calf muscles.

Causes of Calf Muscle Tears
Overload: Increasing the weight on a calf raise machine too fast. You can just imagine if you jump from 40kg to 60kg in one week. The muscle won’t be able to keep up.
Inadequate warm-up: A sudden contraction like a jump or sprint while your calf muscle is not prepared for it, puts you at risk of a muscle tear.
Poor technique: Overpronation of the ankle causes forces to focus over the inside of your calf, which increases the load on the medial head of Gastrocnemius.
Overuse: A sudden change in your interval training, or hill sprints are a dangerous area to venture in. For instance, increasing your pace, distance and frequency all at the same time puts a lot of pressure on your muscles without adequate recovery time.
Overstretch: Running hills or on a incline forces your muscles to contract from a stretched position. A sudden contraction from a stretched position, where muscles are usually weaker, puts your calf muscles under enough strain to shear the fibers.
Weakness:– Muscle fatigue plays a role in runners who are not able to maintain the muscle contraction. Calf muscle endurance and conditioning to be able to handle repetitive contractions of your muscle. When fatigue kicks in, the muscle fails.
Shoes: Poor support for your foot will cause muscle forces to concentrate along the inside of your calf, which loads those muscle fibers more that the outer part. These abnormal forces on the inside of your calf will cause the fibers to fatigue faster and tear first.
How severe is my calf muscle sprain or tear?
If you have a grade 1 muscle tear, where less than 20% of the muscle fibers are torn, you will have no visible bruising and minimal swelling (if any). You might even be able to continue jogging or playing sport, but with pain. You won’t notice any weakness, but stretching your calf, like taking a big step or climbing stairs will be painful. Calf tightness and muscle spasm will be noticeable, but you’ll still be able to walk, drive and go about your normal day.
A grade 2 muscle tear is when 20 to 80% of the muscle fibers are torn. In this case, you will hear a pop or snap when it happens, and then you’ll be unable to continue due to pain. There will be obvious swelling, usually around your ankle, as gravity makes the swelling move towards your foot. In most cases there will be obvious bruising in the area of the muscle tear. You will notice some weakness when you push off while walking, and any movement that stretches your calf muscles will cause a sharp pain. With this grade of injury, you’ll be able to pinpoint the exact spot where your pain is concentrated.
Grade 3 muscle tears are also known as a complete rupture, and is the most severe form of a muscle tear. You will hear a loud pop or snap when the injury happens and won’t be able to put weight on your leg. Swelling will appear shortly after the injury and you will have significant bruising over the injured area. In a complete rupture, you will have severe pain when the muscle is stretched. You won’t be able to stand up on your toes due to weakness and there may be a visible gap in the muscle.
Physiotherapy diagnosis
Our physiotherapists are experts at detecting a muscle tear because we spend up to 8 hours a day working on soft tissue. As they say, “we just have a feeling for it”. We test the range of movement at your knee and ankle, assess the muscle length of Gastrocnemius and Soleus, and use specific muscle tests to determine whether the injured tissue can tolerate load. Getting an accurate history gives us a framework of what kind of injury we’re working with. A thorough clinical assessment allows us to make a diagnose and formulate a rehabilitation program to get you back to tip top shape.

X-rays
In some rare cases we may refer you for an X-ray to exclude any knee or ankle pathology. X-rays only show bones and, therefore, won’t give us an indication of the condition of your calf muscles. These tests will only be necessary if we suspect a tibial fracture or an avulsion fracture with an Achilles tendon tear.
MRI
An MRI is an expensive test and usually unnecessary in an uncomplicated calf muscle strain. However, if we suspect that the interosseous membrane is involved, we may refer you to a specialist for an MRI. Injury to your calf muscles involving this membrane is a serious, but extremely rare problem, which might cause an instability between the two bones in your lower leg.
Why is the pain not going away?
When a muscle tears, your body attempts to repair the injured fibers by sending cells to reattach the torn ends of the muscle fibers. This process is very similar to how your body repairs an open skin wound, like a cut on your finger. If you keep on picking at it, you will shear away the new cells necessary for healing. The same thing happens when you walk or run through the pain of your torn calf muscle. Ignoring the problem just gets you stuck in an endless loop of muscle damage with no time to heal.
You may decide its a good idea to ‘rest your calf’, so you take a few days off. Eventually the pain in your calf goes away (usually 3 days), but when you try to run, the pain is there waiting for you. If the muscle length and strength is not restored, you will rip the wound wide open and start from the beginning again. This is the most common reason why patients consult us, because they get stuck in this cycle of repair and breakdown.
Scar tissue is like a scab forming over a wound on your skin. The scar needs to form in the same direction as the muscle fibers, and have the same length and tensile strength of the surrounding tissue. When you keep walking or running through the pain, you’re ripping the wound wide open again. This vicious cycle eventually leads to poorly formed, thick scar tissue, like a dense web of scattered fibers that restricts the normal sliding of the muscle fibers. You won’t fix the dent in your car without having it smoothed, polished and painted, so why don’t you go through the same trouble for your calf?

Problems we see when patients come to us with calf pain
Deep vein thrombosus (DVT)
DVT is an uncommon, but potentially dangerous complication after a calf muscle tear. This happens because your calf muscles act as a “muscle pump” to circulate blood from your lower legs back to your heart. If you have a pulled calf muscle, you might avoid using the muscle due to pain. The result is decreased circulation in your leg which increases the risk for developing a DVT. Signs to look out for are warmth and redness of the skin over your calf and extreme pain when you try to stretch your calf.
Nerve entrapment
The normal healing process after a calf muscle strain involves the formation of scar tissue. This scar tissue is supposed to knit together the torn muscle fibers, without interfering with the surrounding soft tissue. A big problem we see after torn calf muscles is nerve entrapment caused by abnormal scar tissue formation. More than one nerve runs through your calf towards your ankle. After a tear in one of your calf muscles, the newly formed scar forms adhesions to the nerves in the area. These adhesions restrict the normal gliding movement of nerves, leading to pain, numbness and paresthesia (pins ‘n needles).
Recurring strains
Another common complication after a calf injury is future calf injuries. This may sound obvious, but very few people realize that healing and recovery are not the same. Healing is part of life, and our bodies are extremely good at healing all sorts of aches and pains. However, this only means that there’s scar tissue where the tear used to be. As part of the process, this new scar tissue restricts movement in the early stages of healing to protect itself. The problems start when you don’t need this restriction anymore. Now you’re stuck with a permanent knot in your calf muscles, and as soon as you push yourself past that limit, you end up with an injured calf again.
Stiff ankles
A complication that usually only ends up at our door some years after a pulled calf muscle is stiff ankles. Your calf muscles are responsible for plantarflexion of your ankle, but there’s another movement that goes hand-in-hand with pointing your toes. That movement is dorsiflexion, which is the opposite of plantarflexion. A tight calf muscle, will keep your ankle in a pointed position, thereby limiting dorsiflexion. Early on, this restriction is small enough that you won’t notice it. Unfortunately, this limitation gets worse over time, until you notice that you always need to climb up a step with the other leg first or you can’t really go down into a deep squat anymore. By then, there’s a lot of work to be done to restore the range of movement in your ankle.
Physiotherapy treatment

Although rest feels helpful in the early days after your calf muscle tear, too much rest leads to a basket of other problems like joint stiffness, muscle weakness, tightness and impaired proprioception.
Your physiotherapist is an expert when it comes to guiding you in finding the balance between rest and activity. The key is load management, not taking all the load away. In the first week after your injury, this means doing as much as you feel comfortable with and not pushing through pain. This will include exercises, like gently moving the joints around your knee and ankle.
As medical professionals, physiotherapists have a wide range of treatment modalities and techniques to help you through each phase of healing. These include modalities like dry needling, ultrasound and laser to stimulate healing, strapping to protect the injured muscle, soft tissue mobilization and myofascial release to treat tightness and restrictions and, of course, exercise therapy to make sure the new muscle fibers are prepared for your day to day activities.
Phases of rehabilitation

Days 1 – 7: Protecting the injured tissue
In this stage of treatment our main goal is to create a “safe space” for you torn calf muscle to heal. This can include walking with crutches and, in severe cases, a moon boot or brace to limit ankle movement. From a physiotherapy treatment side, we will use various techniques and modalities to stimulate healing, without disturbing the fragile, new muscle fibers.
By the end of this phase your pain should start diminishing, and you should be able to tolerate some weight on your foot.
Weeks 2 – 3: Regain Range of Movement
The most important component of calf muscle strain treatment is regaining full range of movement. This stage of treatment overlaps with the first and stars within the first week after injury. As the muscle heals, we must make sure that the scar tissue lengthens to prevent future restrictions. To achieve this, we use myofascial release, range of movement exercises and nerve mobilization.
By the end of this phase, you should have at least 50% of the movement compared to the uninjured side. You will still have pain, but will notice that the intensity is lower. By now, you should also be able to take weight on your foot without the sharp, stabbing pain.
Weeks 3 – 6: Eccentric strength
A muscle contraction works in two directions: One where the calf muscle shortens like a heel rise (concentric), and the other type of contraction controls the descent (eccentric). Eccentric loading is especially important when in muscle strain treatment, because it loads your calf muscle fibers while being lengthening. These type of exercises is vital at conditioning the muscle fibers to absorb a force.
At the end of this stage you should be walking without crutches and taking almost full weight on the injured side. You should also be able up and down a step without switching to the uninjured leg all the time. Pain should be minimal, and is usually replaced by a feeling of muscle tightness at the end of phase 3.
Week 4 and onwards: Concentric Muscle Strength
Shortening of the muscle during a contraction involves resistance exercises that will be progressed gradually as healing takes place. We will monitor strength throughout the whole rehabilitation process, to determine if and when we can increase the load on your calf muscle. Exercises will start becoming more challenging during this phase, to build strength and endurance.
By the end of this phase, you should be walking normally and have no pain with day to day activities. You can still feel some discomfort or mild pain during or after exercises, as the new muscle fibers adapt and change to handle the load. You should be able to start jogging on level surfaces and have about 90% of the movement of your uninjured calf.
Weeks 6 – 8: Full return to activity
Your calf muscles must be tested under higher load and speed to ensure that the muscle will be able to keep up with the demands of your body. During this phase, your physiotherapist will continue to monitor your calf muscle, as you start adding more challenging activities to test the muscle’s response to different forces.
When you reach this phase of treatment, you should have full range of movement when stretching your calf and be climbing stairs without a limp. You should also be jogging and be able to jump and change direction without hesitation.
Healing time
Calf muscle strains usually need 4-6 weeks to heal, depending on the severity. Return to sports participation will take longer and should not be confused with the healing period. This is guided by the medical professional treating you to ensure you’re safe to put your calf muscles and surrounding structures under stress.
The amount of sessions required depends on the severity of the calf strain and your cooperation with the advice we give you. Every person is unique, so it varies. In most cases we need to see you twice a week for the first two weeks, then one treatment session for the next two weeks, increasing the interval length between each session as we progress until you’ve made a full recovery.
Other forms of treatment
- Your doctor can prescribe medication for pain management.
- In the final stages of rehabilitation, a biokineticist can assist you with a training program to get you back to your sport.
- An ankle brace or moon boot may be useful for pain relief in the acute phase, depending on the severity of your calf muscle tear.
- Crutches are quite helpful in the days after the initial injury, to help with pain relief and protect your torn calf muscle.
- A stretching practitioner is not recommended in the first weeks after a calf muscle strain. Stretching too early will prolong recovery and cause more damage.
- Massage is also not recommended unless cleared by your physiotherapist. This would depend on your phase of healing.
- Foam rolling will cause further damage, and should be avoided until your physiotherapist tells you otherwise.

Is surgery an option?
Non-surgical treatment like physiotherapy is the first choice when it comes to torn calf muscles. However, surgery would have to be considered for an Achilles tendon rupture. This type of injury is on the severe side of the scale, and the hard work begins after surgery. Rehabilitation after an Achilles tendon repair can take up to 9 months or a year.
What else could it be?
- Achilles tendinosis or tendinitis: Tendinitis will normally be painful at rest, go away during activity and return after cool down.
- Flexor Digitorum Longus muscle tear: This injury will cause pain more localized to the ankle and foot, especially bad when taking weight on the affected side and cramping of your foot.
- Shin Splints: This is when the deeper Soleus muscle tears away from your shin bone, and the pain is usually felt more at the front of your lower leg.
- Posterior Compartment Syndrome: You will have pain during exercise, which goes away completely with rest.
- Posterior Tibial nerve entrapment: Symptoms of entrapment include cramping, pins and needles, burning sensation along the calf or ankle.
- Gastrocnemius or Soleus muscle cramp: Cramps are sudden, painful, involuntary contractions of the muscles due to overexertion, dehydration, dietary insufficiency or decreased flexibility.
- Deep Venous Thrombosis (DVT): A warm, red, swollen calf may be a sign of a DVT.
Also known as
- Pulled calf muscle
- Torn calf muscle
- Gastrocnemius tear
- Soleus tear
- Calf strain