Shoulder joint pain is very disabling. What sets us humans apart from the rest of the animal kingdom is our opposing thumbs. Your shoulder “gives your thumbs wings” because it enables you to move, manipulate and bring closer what you have in your hands. Without a mobile shoulder you will not be able to wash your hair, hang the laundry or do a push up. Changing gears or getting dressed can become painful, when you neglect your shoulder joint pain.
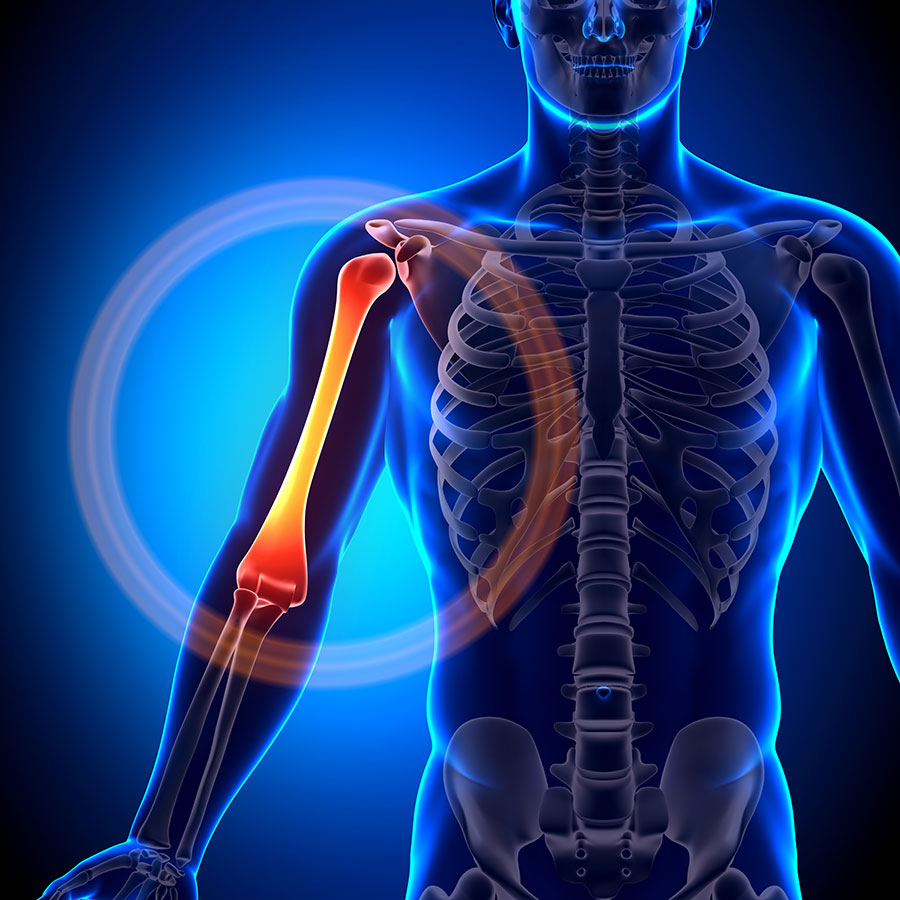
Anatomy of the shoulder joint
The shoulder is actually a team of joints that control the movement of your arm. The main joint of the shoulder is the glenohumeral joint, which is a ball and socket joint, similar to the hip. A ball and socket design allows circular movement of the arm in all directions. The acromio-clavicular joint connects the collar bone to the shoulder blade and the sterno-clavicular joint connects the collar bone to the breast bone. Small gliding movements from these two joints, which you don’t even have to think about, increases the range of motion of the shoulder.
The socket is shallow, to give you great mobility, but offers little stability. Fibrous tissue that attach to the edge of the socket, the glenoid labrum, increases the depth of the socket. Articular cartilage lines the inside of the ball and socket joint. It absorbs shock and compressive forces, like catch and throw of a medicine ball. The cartilage allows the joint to move freely without friction. The cartilage in the shoulder is thinner than in weight bearing joints like the hip.
Injury to the joint, glenoid or cartilage causes painful shoulder joint movements. When a “simple joint sprain” remains inflamed, the bone or cartilage is likely injured.
A synovial membrane lines the joint, almost like insulation. This membrane secretes a fluid (synovial fluid) that lubricates the joint like oil in a car’s engine. The joint capsule (ligaments that surround the joint) covers the synovial membrane.
The shoulder joint is the most mobile, but least stable joint in the body, therefor dislocations happen easier than with other joints. Because the shoulder joint can move in all directions it has limited passive stability (provided by ligaments). When dynamic stability (provided by muscles) is poor, extra stress is placed on the shoulder joint.
What does the shoulder do?
I know! Pick me! Did you image raising your arm to answer this question? Your shoulder does that. Your shoulder allows movement, be it gracious like a ballerina or ferocious like a boxer. You need shoulder mobility to reach up high and shoulder stability to control movement of the elbow and hand, like playing piano or doing a push up. You also need shoulder strength and endurance if you have a physical job, that includes carrying the kids too.

How does a shoulder injury happen?
Any or all of the structures that make up the shoulder joint can be injured. Strains, sprains, ruptures and dislocations can cause small tears in the ligament, joint capsule, glenoid labrum or articular cartilage. In an attempt to heal these tears inflammation forms in the area. Inflammation is necessary for healing. It acts as the body’s ambulance service to get everything needed to the area. The shoulder joint is a small space, inflammation takes up a lot of room. This may cause sounds from the shoulder joint on movement or a feel like sand in the joint.
Ignoring even a slight shoulder injury can have long term effects, because compensatory movement patterns form in the blink of an eye. Moving non optimally strains structures unnecessarily and can cause pain. Rather have your shoulder joint problem sorted out.
What causes a shoulder joint injury?
Shoulder joint injuries are classified as acute (3 months) or chronic (longer than 3 months). Shearing or tearing forces cause acute shoulder joint injuries. This happens when the shoulder joint dislocates (complete separation of the ball and socket) or subluxates (partial separation of the ball and socket). Degenerative joint diseases cause chronic shoulder joint pain. Like whaat happens with osteo-arthritis (OA) of the joint, the articular cartilage changes.
Causes of shoulder joint pain:
- Degenerative changes, eg. Osteo-artrithis (OA), auto-immune diseases (Rheumatoid arthritis), Diabetes Mellitus, smoking or osteoporosis.
- Over-use/repetitive strain injuries: Micro-trauma from repeated loading or compression of the cartilage as the joint surfaces glide over each other, eg. increase in training load, new exercises, wrong form when exercising.
- Traumatic injuries, eg. falling on the arm, an unexpected traction force, shoulder dislocations/subluxations or fractures.
- Post traumatic OA can occur in young people who suffered a severe shoulder injury or had surgery.
Why do the shoulder joints ache after an injury?
With an acute injury, the articular cartilage, synovial membrane, bone or the joint capsule can be damaged. The strain on the tissue cause inflammation and swelling inside the joint. The swelling increases pressure inside the joint, and thereby causes more compression. Bleeding from injured blood vessels may increase pain. This increase in pressure irritates the nerve endings in the area.
Age related degeneration (OA) causes chronic shoulder joint pain. The arthritic shoulder has thinned articular cartilage. The damaged cartilage doesn’t cause pain as it has no nerve endings. The pain is felt when the bones touch.
Damaged cartilage can react in two ways. First, it can produce new cartilage, but it may not be as smooth as before. The new cartilage is often bumpy and irregular. This causes painful shoulder movements. Secondly, the bone may form growths, known as a bone spur or an osteophyte. This will increase the friction inside the joint and cause in pain in the shoulder joint.
Symptoms of degenerative shoulder joint pain (OA)
- Pain: Movement increases pain, rest decreases pain. Pain, tenderness and stiffness is worse in the mornings, after inactivity or in cold weather. Night pain may disrupt sleep.
- Swelling: Is seen in acute articular damage, but is rarely seen in osteoarthritis. OA is not an inflammatory disease (there is no inflammation) it is mechanical (bone on bone contact) but in rare cases can be red or feel warm. Compression injuries in the articular cartilage does tend to swell.
- Stiffness and loss of movement: In chronic conditions the limitation in movement gets worse with time. Joint deformities can develop with the wear of the cartilage.
- Sounds: Movement can cause crepitus (popping, crunching or scrapping sounds). It may feel like sand in the joint, this indicates joint surface irregularity.
- Locking: Movement of the shoulder is blocked. This may cause sharp pain when you move. You cannot take the arm up high above the block or catch.
- Muscle wasting and weakness: Painful shoulder movements will make a person avoid movement. This causes muscle atrophy.
Diagnosis
X-ray
X-rays show the bones (not the soft tissue) and is ideal to show us what is going on inside the joint. X-rays are taken when you have a painful shoulder joint but might not show small defects if the angle is incorrect. We will refer you for X-rays if we suspect OA, fracture or dislocation.
Sonar
Sonar (Diagnostic Ultrasound) show soft tissue (muscles, ligaments and nerves) and is therefor not ideal if we suspect a shoulder joint injury. A sonar would show the depth, length and direction of a muscle tear, but has a limited use in shoulder joint issues except for a shallow joint like the acromio-clavicular joint.
How we test for a shoulder joint injury
- Physiotherapists are able to test and determine if the cause of your pain is from the muscle, joint, ligament or nerve. This is known as a clinical assessment.
- Joints are tested in their ability to move freely without restriction. A joint can be moved actively (meaning you voluntarily move the joint without assistance) or passively (meaning the therapist move it for you while you relax). The passive movement test will exclude the injury from muscles and allow us to assess the joint independently.
- The joint will be compressed (surfaces pushed into each other), distracted (pulled away from each other) and moved to the end of the range while in the control of our experienced physiotherapists. This will allow us to determine the integrity of the joint while we feel for smooth movement and listen for sounds from the joint.
Why is my shoulder joint pain not going away?
The shoulder is often plagued by referral pain, which makes it the victim of pain, not the culprit. We have seen numerous patients that suspect their shoulder is the cause of their pain, but after our assessment we find that the pain is caused by a different structure. A neck disk injury can cause pain that travels from the neck to the shoulder.
We often treat shoulder joint pain after previous surgery or old neglected injuries. The patient feels that the pain never goes away, but it might be a complication. Rehabilitation, if done properly, will prevent long term joint pain, like post-traumatic osteoarthritis. General exercise programs are sufficient for ankle injuries, but it takes specialised knowledge to rehabilitate a shoulder. Shoulder pain can debilitate all activities you do with your hands and that is why very specific rehab is required from a professional who knows the shoulder in and out.

Physiotherapy for shoulder joint injuries
Initial phase treatment
- Early injury treatment follows the PRICE protocol – Protect (deload or immobilize), Rest, Ice, Compress and Elevate.
- Avoid harming activities – Repetitive movements, overuse or taking anti-inflammatories too early.
- Brace or Support – A sling or strapping
- TENS machine – Controls pain with electrical nerve stimulation.
Intermediate phase treatment
- Subacute soft tissue treatment
- Joint mobilisations
- Kinesiology Tape
- Supportive Taping & Strapping
- Laser treatment
- Ice / Heat Packs
- Medications
- Loading through safe range, exercises
Final phase treatment
- Foam roller
- Stretching exercises
- Strength exercises
- Closed kinetic chain exercises
- Eccentric exercises
- Proprioception & balance exercises
- Agility & sport specific exercises
Other factors to consider
- Biomechanical Analysis
- Joint Mobilisation Techniques
- Video Analysis
- Prehabilitation

Physiotherapy treatment goals for shoulder joint pain
- Decrease pain and muscle tension (pectorals, upper trapezius and levator scapulae muscles) in the shoulder, neck and shoulder blade to achieve optimal alignment for movement.
- Change poor shoulder position to move more naturally.
- Increase strength of the muscles that stabilize and move the shoulder (serratus anterior and the rotator cuff muscles).
- Regain joint positioning sense and normal movement.
Both nonoperative rehabilitation and postoperative rehabilitation of shoulder muscle injuries involve the following principles:
- Deloading of the affected muscle and rehabilitation of the whole area.
- Prevent trick or compensatory movements, like lifting the shoulder before moving the arm.
- Improve muscular strength and endurance.
- Ensure free movement of the joints above and below the shoulder, the neck and elbow.
- Restore normal movement patterns.
- Increase mobility of the tissues to allow normal movement.
Recovery time
Shoulder pain has many causes and EARLY diagnosis and treatment is the best way to recover fully and quickly.
Shoulder joint pain will start to improve within two weeks after your injury, if you manage your injury properly. However, joint pain is complex and will be managed according to how severe the injury is. Generally shoulder joint pain recovers within 8 to 12 weeks. The time can vary greatly as it depends on both the nature of your injury and the treatment plan that you develop with your physiotherapist.
Degenerative conditions do not recover fully as it is a progressive process. The goal here is to reduce the speed at which it gets worse and reduce the number & length of a flare up. The sooner we assist you in managing the condition the better the long term results are.
Medical management
Physiotherapy, not surgery, is the best treatment to start with for a shoulder joint injury. In addition to physical therapy, non-surgical treatment may include anti-inflammatory medication and steroid injections. Steroid injections are commonly used in shoulder joint treatment. These treatments are prescribed by a sports physician.
You may need a sling or brace to limit movement for a little while. An orthotist will fit you for a sling.
How can you prevent recurring shoulder joint pain?
If you have suffered from shoulder pain in the past, you are unfortunately more likely to suffer in the future. The most common cause of recurrent shoulder pain is insufficient rehabilitation. If you have had a severe shoulder injury or previous surgery you are at risk of secondary trauma related joint degeneration.
We will create a shoulder joint treatment plan to decrease the pain and to prevent it from coming back. The effort you put into the treatment help determines how fast and how good the recovery will be. There are no guarantees that you will never have a shoulder injury again, but active people who exercise, reduce the risk of developing shoulder pain.
Discuss with your physiotherapist the specific postures and activities that you perform on a daily basis. They will aim to help you to understand how to position yourself and move with the lowest risk of injury based on your unique circumstances.
When is shoulder surgery necessary?
After a consultation we can assess the need and possibility of surgical intervention. You will be referred to a specialist if it is in your best interest.
- Significant tendon and muscles tears (grade III – full ruptures) can often require surgical repair
- Damage to the shoulder joint itself and the labrum (such as a SLAP lesion or Bankart’s lesion)
- Patients that have suffered a severe dislocation, or recurrent dislocations of the shoulder joint
- Patients with chronic degeneration of the shoulder joint surfaces
The type of surgery performed will determine the recovery time and management strategy determined by your orthopaedic surgeon. Our extensive experience in rehabilitating shoulder injuries post-surgery means that we can work to get you pain free in the shortest and safest possible time. We tailor a sport specific rehabilitation program to get you back to where you want to be.
What else could the pain be?
- Acromioclavicular injury
- Glenoid labrum tear : Slap lesion, Bankart lesion
- Cervical pathology: Cervical nerve root injury, Cervical Radiculopathy, Cervical Spondylosis
- Subacromial Impingement
- Osteoarthritis, Rheumatoid Arthritis
- Shoulder Instability
- Subscapular nerve entrapment
- Scapulothoracic bursitis
- Adhesive Capsulitis
- Biceps Tendonitis
- Calcific Tendonitis Shoulder
- Thoracic Outlet Syndrome
- Glenohumeral ligament tears or sprains
- Subluxation or Dislocation



